
Provocative Idea:
Bench, Bedside, Curbside, and Home: Translational Research to Include Transformative Change Using Educational Research
Emily Hahn
University of North Dakota, UNITED STATES
Emily.hahn@und.edu
Translational research originated in the medical field during the 1990s to describe taking discovery based research through the steps of applying it to clinical research and patient-oriented care. This model is implicitly linear, depicting the flow of information from researchers’ bench, to a clinical trial bedside, to a primary care physician’s practice. The prevailing model of translational research, referred to as “Bench to Bedside to Curbside,” is limited in that it does not adequately incorporate stakeholders outside of the professional or research community because Curbside refers to physician care delivered to patients. This omits the transformative impact that research can have on the general populace if implemented through educational research, disseminating knowledge to people who can use it. In this article we argue that a fourth category needs to be incorporated into the previous T1-T3 Bench to Bedside to Curbside model, and this fourth category represents T4, “Home.” We seek to further define and describe, while providing a new model for translational research that is more circular in nature and inclusive of the general populace. We also suggest that the incorporation of educational researchers and practitioners would expand the current collaborative nature of translational research and is a way to expand the translational model. This promises more adequate, effective, and sustainable impacts on a target population.
Index Terms: translational research; educational research; transformative change; surface learning; deep learning; inquiry based learning
Suggested Citation: Felege, C., Hahn, E., Hunter, C., & Gleditsch, R. (2016). Bench, bedside, curbside, and home: Translational research to include transformative change using educational research. Journal of Research Practice, 12(2), Article P1. Retrieved from http://jrp.icaap.org/index.php/jrp/article/view/548/453
Translational research emerged as an attempt to fill the gap between researchers and practice. The term originated in the medical field during the 1990s to describe the process of taking basic research through the steps of applying it to clinical research and patient-oriented care (Westfall, Mold, & Fagnan, 2007). In the field of medicine, translational research has been defined as “the process of applying ideas, insights, and discoveries generated through basic scientific inquiry to the treatment or prevention of human disease” (National Institute of Neurological Disorders and Stroke, 2008). This type of research has placed emphasis on taking discovery-based science from “Bench to Bedside to Curbside.” In medical science this research model is represented as T1-T3 where the T stands for Translational and T1 is the Bench, T2 is the Bedside, and T3 is the Curbside (Dankwa-Mullan et al., 2010; Mata & Davis, 2012; Westfall, Mold, & Fagnan, 2007). While translational research was first used in the area of cancer research in the early 1990s, it has since been refined and applied to a number of fields (Emmert-Buck, 2014). An example of this is the “lab to land” example in agricultural research (Dash & Ulrich, 2014). The National Institute of Health (NIH) in the United States has been a central driver of the development and proliferation for this term, each year spending billions of dollars on biomedical research aimed mostly at understanding how living organisms work (Westfall, Mold, & Fagnan, 2007). NIH funding for translational research is generally aimed towards the attempt to streamline and improve the monumental task of taking newly discovered treatments and medications into effective clinical practice (Westfall, Mold, & Fagnan, 2007).
A key feature of translational research is its multifaceted and highly interdisciplinary nature, due to the magnitude of challenges facing such a process (Emmert-Buck, 2014; Rajan, Sullivan, Bakker, & Van Harten, 2012). Yet, despite all of the work and funding placed towards translating basic research and discovery based science into effective clinical practice, there are still significant shortcomings in the delivery of effective acute and long-term care and tremendous room for improvements in preventive medicine (Westfall, Mold, & Fagnan, 2007).
Very little work has addressed the movement of research beyond the professional medical community. Within translational research, the actuality of disseminating and transforming must be in a way that positions the general populace as more than a passive recipient of the benefits of such work, in turn addressing one of its serious limitations. This limitation results in the omission of a fourth and critical component of translation research, which we propose would represent a T4 step, which we propose to call “Home.” There are very few works that make any reference to T4, and those that do address it only abstractly as “real world” application (Khoury et al., 2007; Rajan et al., 2012). According to Khoury et al. (2007), real world refers to the translation of controlled clinical trials to population health impacts by the adoption of evidence-based recommendations. Rajan (2012) explicates translational research as a continuum that covers basic research through practice yet ends without any explanation beyond practice or a medical-centric focus. However, this tells us little about what real world actually means in reference to translational research. We wish to expand and redefine the concept of T4 to mean Home, where translation encompasses transformative behaviors resulting in a sustainable impact on actual outcomes for the target population.
Currently, the concept of Bench to Bedside to Curbside is missing a critical fourth step that prevents the existing models from being truly translational. This fourth and critical step is our defining piece (Home) and necessitates the inclusion of educational researchers and practitioners that results in a transformative change. We also contend that the interdisciplinary nature of translational research must be further expanded to place a greater emphasis on the inclusion of such transformative change.
We begin with a consideration of the linearity of the T1-T3 model as a whole which represents a generally one-way, top-down flow for the development and dissemination of knowledge, wherein the ultimate source of knowledge is currently represented as basic research. The linear movement of information between stages is not what we critique, but rather the lack of a mechanism providing feedback between stages to address unintended consequences or negative outcomes. Such models can be perceived as exclusionary by the general populace because they disregard how novel learning can be generated at any level of the translational model.
Furthermore, we propose that there should be a source for collecting information at each level of the Bench to Bedside to Curbside to Home model. By including educational researchers who are trained at gathering information from participants and utilizing that information to modify practice, we propose that it is possible to improve the T1-T3 model through inclusion of the T4 step. Translational research requires a more circuitous and inclusive means, in turn, providing mechanisms to progress from the Home population and feed back into each level of the model. The current conceptual framework of translational research involves stakeholder input, but the focus on this input has been placed on data gathering or changes in practice and policy centered around a healthcare provider rather than general community members (Mata & Davis, 2012). Limitations that have previously been addressed identify the fact that translational research fails to incorporate or address the practical concerns of stakeholders (Dash & Ulrich, 2014).
Finally, the already broad and collaborative nature of translational research needs to expand to include educational researchers and practitioners who are already proficient at taking discovery based science and making it applicable or relatable to a broader audience. This puts educational researchers in a unique position to offer their expertise in translating basic research and providing feedback between each step in the T1-T4 model. Consistent collaboration with educational researchers would facilitate better assessment and outcomes for the general population, which would increase the likelihood of further empirical studies, related to translating practice-based research that engage the target population.
The Bench to Bedside to Curbside model has compartmentalized the implementation of new knowledge, mechanisms, and techniques under translational research into three categories described as T1, T2, and T3 (Dougherty & Conway, 2008; Woolf, 2008). Basic science and it’s testing in clinical practice has been recognized as the first step in this process (Dougherty & Conway, 2008). For example, T1 would represent laboratory work that led to a new understanding about the mechanism of a disease and would be translated into a new diagnostic method, therapy, or prevention, and subsequent initial testing (Woolf, 2008). This initial testing would seek preclinical animal research and use that to guide Phase 1 and Phase 2 clinical trials (Westfall, Mold, & Fagnan, 2007).
Following these first tests, T2 focuses on creating more patient-centered evidence of clinical effectiveness in an effort to determine who benefits from clinical care. T2 seeks to take Phase 3 clinical trials with controlled observational studies to deliver the right care at the right time to the right patients (Westfall, Mold, & Fagnan, 2007). This was traditionally done through outcome-based research, health service research, and work examining comparative effectiveness (Dougherty & Conway, 2008). Research classified as T2 has a common theme around moving research from clinical studies into broader practice in community and ambulatory care settings, typically focused on primary care (Mold & Peterson, 2005).
The third category of the T1-T3 model of translational research was originally suggested by Westfall and colleagues who recognized a shortfall with previous translational models that were limited to T1 and T2 (Woolf, 2008). This expanded model, described a third step, T3, as research related to the dissemination and implementation of practice-based research (Westfall, Mold, & Fagnan, 2007). In their model, T3 sought to ensure that evidence-based treatment, prevention, and interventions are reliably delivered to individuals within the population following clinical trials (Westfall, Mold, & Fagnan, 2007). This category of translational research has focused on work related to the measurement and accountability, implementation, and scaling of health care to improve quality and value (Dougherty & Conway, 2008). We suggest that delivery as an outcome is not enough and therefore another level is needed.
The first group to propose a fourth category of translational research occurred nearly a decade ago when Khoury and coauthors termed “real world” health outcomes as a potential T4, describing an expansion of the translational research continuum (Khoury et al., 2007). However, the context of their work remained in the medical profession within genomic medicine. This illustrates two key points for our proposed model.
First, there is not a clear explanation of what “translational” means because translational research draws upon several fields as a result of the interdisciplinary nature of such work, resulting in terms that are often used inexactly (Emmert-Buck, 2014). We propose a refined definition that places emphasis on transformation, all the way from the Bench, through the Bedside and Curbside, and into the Home. Adding the additional level of Home requires assessing the impacts of research on the actual behaviors and actions of the target population. While various models already developed seek to assess the impacts of translational research upon the target population (Scott et al., 2014) our model proposes that research is not upon people but rather with people. This distinction calls for measuring behavioral change where the impact occurs.
Second, the T1-T3 model remains as a relatively linear model for translational research with implication that the “bench” researchers are at the top, and knowledge flows downhill through cascading events to be translated to the general populace who are represented as passive consumers or recipients rather than active participants in research. This leads to an important goal we are currently working on in providing a mechanism to incorporate the target population into work that is labeled translational.
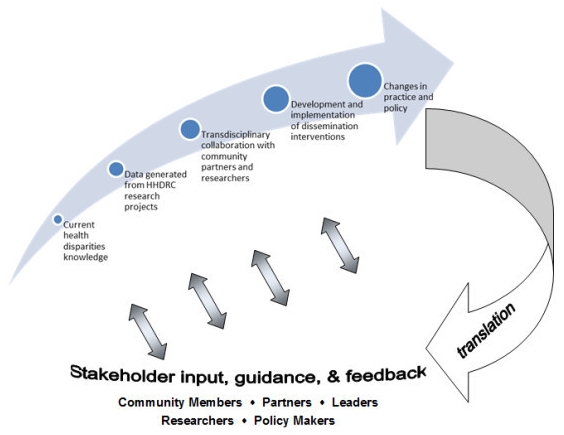
The T1-T3 model of translational research represents a mostly linear flow, though previous authors acknowledge the need for feedback within the system as research findings are tested at successively broader levels. Dougherty and Conway’s (2008) model is linear and it lacks representation of stakeholders. Mata and Davis’s (2012) model (see Figure 1) includes stakeholders throughout, however, it lacks clarity in roles or mechanisms that allow for quality feedback into the translational process.
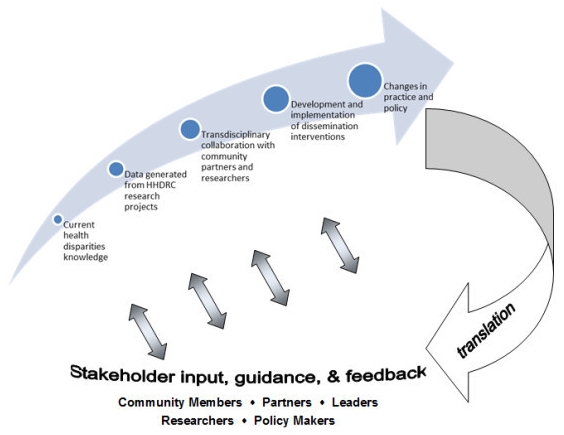
Figure 1. Mata and Davis’s translational model (Mata & Davis, 2012, p. 2, reproduced with permission).
“The ‘practitioners’ who apply evidence in these settings include patients, public health administrators, employees, school officials, regulators, product designers, the food industry, and other consumers of evidence” (Woolf, 2008, p. 212). This is the only significant mention of patients being active participants in this process, rather than passive recipients of knowledge that has trickled down.
Members of the general population need to be actively included as an integral part of any model related to translational research in order for the work to be considered truly translational. This research must be meaningful and understandable to a general population, and there must be mechanisms in place with the primary goal for implementation and genuine change in the availability of education to all individuals in society.
The everyday person does not want to be handed a research article describing to them how to obtain education on translational research or what they need to do to make it available to them. There must be mechanisms in place to convey information from T1-T3 to the stakeholders in a meaningful way. The design of such mechanisms ought to be informed by research on actions, attitudes, behaviors, culture, and thinking of the stakeholders. Educational researchers can assist in the design of such mechanism. Adding these professionals would also enable additional data gathering and publications in primary research outlets that could feed information back to researchers and practitioners at all levels. We propose a model more akin to the one by Dougherty and Conway (2008), although we acknowledge that this model has a disconnect between the linkage of Bedside and Home.
To address the lack of a clear definition and the linearity of current models, educational researchers and practitioners need to be actively incorporated into the already collaborative and interdisciplinary teams involved in research that claims to be translational. This would allow for educational researchers to become involved in changing actions, attitudes, behaviors, and thinking through best-practices in education. Doing so would also provide a direct mechanism for monitoring learning, and subsequent changes or adjustments within the target population by professionals who are specifically trained to do this through education. This would subsequently generate useful results in professional outlets that feed directly back to researchers at the Bench, Bedside, and Curbside.
One illustrative example of ineffective translation may be taken from the medical field. Bradley et al. (2005) critiqued the use of β-blockers, a class of drugs developed in the 1960s, in the treatment of myocardial infarctions, commonly known as a heart attack (Bench). Their effective use in the current treatment of myocardial infarctions was established in the 1990s through a series of clinical trials and the results were well publicized among the medical community (Bedside). Despite this long and well documented history, the administration of this treatment is still not consistent or timely in many cases (Bradley et al., 2005). This lack of effective and consistent implementation is one illustration of a breakdown with the T1-T3 model because the delivery of treatment is not always implemented effectively.
In addition, there is the challenge of current researchers “with limited understanding of and experience with effective methods of engaging communities. Furthermore, limited guidance is available for peer-review panels on evaluating proposals for research that engages communities” (Ahmed & Palermo, 2010). The importance of community-based participatory research has been noted in both health care and education fields:
[Community-based participatory research is a] collaborative research approach that is designed to ensure and establish structures for participation by communities affected by the issue being studied, representatives of organizations, and researchers in all aspects of the research process to improve health and well-being through taking action, including social change. (Ahmed & Palermo, 2010).
A significant benefit of this research design is how community participants then see the long-term gains associated with research (Viswanathan et al., 2004). However, if researchers are not skilled in this type of research design then engaging communities effectively becomes a further challenge.
By applying our proposed expanded model of Bench to Bedside to Curbside to Home, we seek to shift the conversation beyond the immediate care provided during a heart attack, beyond development of theory in education, and beyond the delivery of knowledge to the patient. Instead, our model would seek to prevent such conditions from arising in the first place by not just translating medical jargon to the public but through the transformative change of patient’s responsibility about preventive activities such as diet and exercise (Home). The intended outcome of this additional stage is to have patients transforming the education they receive to initiate and maintain personal change. For example, we propose that preventing the heart attack by fostering a sense of responsibility toward establishing and maintaining personal health through appropriate diet and exercise would be equally, if not more, beneficial than effective treatment during or after the heart attack.
Using the example of the heart attack from above, a primary care physician can tell or even show a patient all of the latest information, data, and research that suggest that diet and exercise can prevent heart attacks (Pattyn, Cornelissen, Eshghi, & Vanhees, 2013). They can discuss treatment options to lower blood pressure and treat symptoms or conditions such as high cholesterol. And they can discuss all of the potential benefits and side effects of potential treatments with their patients. But physicians are not generally trained in educating patients, and many patients, despite the warnings of their doctors, fail to integrate the information they have been provided into their lives in a way that reduces their risk of a heart attack.
We propose that this is at least in part due to the reality that many patients, who are likely to suffer a heart attack are not simply ignoring the information they are provided, but rather failing to transform their lives in a way that results in real changes in health outcomes. We propose that this is the result of surface learning that results in a patient’s ability to regurgitate facts (i.e. that diet and exercise are important to heath), but fails to elicit deep learning which would could alter the behavior and attitude of the patient (i.e. developing, prioritizing, and implementing a healthy diet and regular exercise plan) (Chin & Chia, 2004).
Our T4 model that expands to the Home would seek to develop and instill the motivation and desire in the general population to change current high-risk behaviors such as poor diet or lack of exercise which are known contributing factors to a heart attack. Using educational research, our model proposes that we go beyond merely educating patients about the benefits of exercise, and developing an exercise plan. Our model seeks to develop a sense of value, responsibility, and empowerment in people so that they change their behavior. Adding Home as an additional level would necessitate looking for the change in actions in the target population, not just documenting an awareness of what needs to be changed.
We have identified a critical omission in the T1-T3 model of translational research; that missing step is T4, which we call Home. However, merely identifying and informing the target population about this omission is not enough to make this translational. Simply stopping there only adds to the gap that extends from previous models. We think there is a need to provide a mechanism to take the missing link and improve on previous models. That mechanism is educational research because it allows for the dissemination of knowledge to the target populations and the collection and analysis of meaningful data that can feed back into the previous T1 through T3 levels.
Our argument is built upon two key premises. The first is that the T1-T3 definition of translational research remains both limited to and centered around professional fields, namely those in medicine, as illustrated in the Bench to Bedside to Curbside model. The second is that the above-mentioned limitation prevents participation, limiting access, disregarding, or even excluding the general populace from being active participants in the translational research process.
We argue that to be truly translational, work must go beyond the interactions that are centered on a medical professional. In order to be truly translational, research must lead to meaningful engagements with target communities. With the addition of T4 (Home) the model shifts focus to include the target population in similar ways to community-based research, which allows for a population to address its own health needs and health disparities while ensuring that researchers understand community priorities (Ahmed & Palermo, 2010).
The outcome of T4 (Home) should be measured with an evaluation and monitoring program that establishes a baseline, establishes an transformational change component, evaluates the impacts or changes in the target population, and then offers a way to provide feedback or a mechanism to improve the original research. This is where we see the need for the inclusion of educational researchers and practitioners.
We acknowledge the fact that T4 has been mentioned previously, but that our model extends and develops the real world concept previously proposed (Khoury et al., 2007). They are correct in identifying the need for real-world connections that link basic and discovery based research beyond more than just the scientific community. While these activities are meaningful to researchers and clinicians, in order to be truly translational, the work must be accessible and meaningful to the general population. The gap in the case of historical translational models is a discontinuity from Curbside to Home.
To demonstrate why educational research is a critically needed addition to the success of translational research, consider that the fields of education and cognitive science have provided ample evidence for quite some time that traditional teaching methods such as lecture are not optimal at fostering student retention and subsequent application of knowledge and skills (Dewey, 1910, 1929; Wood, 2009). There is a long and well-established history of calls for reform in education, especially within the science, technology, engineering, and mathematics (STEM) disciplines. The report, A Nation at Risk; The Imperative for Educational Reform, published by the National Commission on Excellence in Education called for significant reform to K-12 science education (Gardner, 1983). The American Association for the Advancement of Science (AAAS) report on literacy goals in science, mathematics, and technology, Science for All Americans also called for similar reforms (Rutherford & Ahlgren, 1990).
Such calls for reform in education led to a number of initiatives to transform how science is taught at many levels of the American educational system. These reforms tended to transition away from simple regurgitation of basic facts that were generally limited in value to the context of the course, and more toward skills that would be valuable and applicable more broadly. One example is Workshop Biology, which was started in the 1990s at the University of Oregon. This model sought to contextualize the importance of a basic understanding of biology by getting students to confront more complex social issues with a biological basis such as vehicle selection, diet and food consumption, child-bearing, and voting in relation to environmental issues (Udovic, Morris, Dickman, Postlethwait, & Wetherwax, 2002).
The model of Workshop Biology was foundational in the development of a more broadly termed inquiry based learning, which focuses on the nature and process of science rather than the memorization of facts (Derting & Ebert-May, 2010). Inquiry based learning has been shown to improve student learning and retention, in general because it makes students active partners in their own education and involves them in the construction of their own knowledge (Freeman et al., 2014).
More recently, the application of new knowledge about teaching and learning has led to the development of spaces specifically designed to engage students in active learning processes. One such initiative that has shown promising results in the areas of active learning includes SCALE-UP (Student Centered Active Learning Environment for Undergraduate Programs) (Beichner, 2008; Beichner, Saul, Allain, Deardorff, & Abbott, 2000). Such strategies have been shown to improve the learning of female and minority students even more than their traditional white male counterparts (Preszler, 2009).
By expanding and building upon the T1-T3 model of translational research, and incorporating educational researchers and practitioners, we propose a mechanism for expanding translational research into a more meaningful endeavor that incorporates the public as stakeholders. Within the healthcare system, this process could link health care providers with a health care delivery system in an effort to optimize the outcomes of health care (Donaldson et al., 2008). This follows the T1-T4 model developed and described above, which represents a more circular mechanism for translational research. The incorporation of educational researchers and practitioners into the multidisciplinary teams of translational research also allows for data gathering and monitoring that can be used in the publication of primary literature to direct and guide research at all previous levels, including Bench, Bedside, and Curbside, and represents a significant move forward by seeking to actively involve stakeholders from a target population. Appropriate translation of cutting edge science to applied problems, delivery to a broad audience starting in the K-12 education system, then continuing through colleges and universities could improve this by getting more people to see the value of science in real life contexts making it more concrete and applied for them. Hopefully such changes will lead to increased awareness and involvement by a broader audience from within the general population through improvements to the dissemination of knowledge in a manner that is closer to home for many people.
Ahmed, S. M., & Palermo, A. S. (2010). Community engagement in research: frameworks for education and peer review. American Journal of Public Health, 100(8), 1380-1387.
Beichner, R. (2008). The SCALE-UP Project: A student-centered active learning environment for undergraduate programs. An invited white paper for the National Academy of Sciences.
Beichner, R. J., Saul, J. M., Allain, R. J., Deardorff, D. L., & Abbott, D. S. (2000). Introduction to SCALE-UP: Student-centered activities for large enrollment university physics. Educational Resources Information Center, Office of Educational Research and Improvement, US Department of Education.
Bradley, E. H., Herrin, J., Mattera, J. A., Holmboe, E. S., Wang, Y., Frederick, P., . . . Krumholz, H. M. (2005). Quality improvement efforts and hospital performance: Rates of beta-blocker prescription after acute myocardial infarction. Medical Care, 43(3), 282-292.
Chin, C., & Chia, L. G. (2004). Problem‐based learning: Using students’ questions to drive knowledge construction. Science Education, 88(5), 707-727.
Dankwa-Mullan, I., Rhee, K. B., Stoff, D. M., Pohlhaus, J. R., Sy, F. S., Stinson Jr, N., & Ruffin, J. (2010). Moving toward paradigm-shifting research in health disparities through translational, transformational, and transdisciplinary approaches. American Journal of Public Health, 100(Suppl. 1), S19-S24.
Dash, D. P., & Ulrich, W. (2014). Ten years of connecting researchers. Journal of Research Practice, 10(1), Article E1. Retrieved from http://jrp.icaap.org/index.php/jrp/article/view/451/344
Derting, T. L., & Ebert-May, D. (2010). Learner-centered inquiry in undergraduate biology: Positive relationships with long-term student achievement. CBE-Life Sciences Education, 9(4), 462-472.
Dewey, J. (1910). Science as subject-matter and as method. Science, 31(787), 121-127.
Dewey, J. (1929). The sources of a science of education (Vol. 17). New York, NY: Horace Liveright.
Donaldson, N., Horn, S., Edwards, J., Miller, G., Gassaway, J., Belden, G., & Hagan, M. (2008). Evaluating the impact of partnerships to improve clinical quality. Joint Commission Journal on Quality and Patient Safety, 33(Suppl. 1), 27-36.
Dougherty, D., & Conway, P. H. (2008). The ‘3T’s’ road map to transform US health care: The ‘how’ of high-quality care. Journal of the American Medical Association, 299(19), 2319-2321.
Emmert-Buck, M. R. (2014). Translational Research: From biological discovery to public benefit (or not). Advances in Biology, 2014, Article ID 278789.
Freeman, S., Eddy, S. L., McDonough, M., Smith, M. K., Okoroafor, N., Jordt, H., & Wenderoth, M. P. (2014). Active learning increases student performance in science, engineering, and mathematics. Proceedings of the National Academy of Sciences, 111(23), 8410-8415.
Gardner, D. P. (1983). A nation at risk: The imperative for educational reform: An open letter to the American people (Report). Washington, DC: National Commission on Excellence in Education.
Khoury, M. J., Gwinn, M., Yoon, P. W., Dowling, N., Moore, C. A., & Bradley, L. (2007). The continuum of translation research in genomic medicine: How can we accelerate the appropriate integration of human genome discoveries into health care and disease prevention? Genetics in Medicine, 9(10), 665-674.
Mata, H. J., & Davis, S. (2012). Translational health research: Perspectives from health education specialists. Clinical and Translational Medicine, 1(1), 1-6.
Mold, J. W., & Peterson, K. A. (2005). Primary care practice-based research networks: Working at the interface between research and quality improvement. Annals of Family Medicine, 3(Suppl. 1), S12-S20.
Pattyn, N., Cornelissen, V. A., Eshghi, S. R. T., & Vanhees, L. (2013). The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome. Sports Medicine, 43(2), 121-133.
Preszler, R. W. (2009). Replacing lecture with peer-led workshops improves student learning. CBE-Life Sciences Education, 8(3), 182-192.
Rajan, A., Sullivan, R., Bakker, S., & Van Harten, W. H. (2012). Critical appraisal of translational research models for suitability in performance assessment of cancer centers. The Oncologist, 17(12), e48-e57.
Rutherford, F. J., & Ahlgren, A. (1990). Science for all Americans. New York, NY: Oxford University Press.
Scott, C. S., Nagasawa, P. R., Abernethy, N. F., Ramsey, B. W., Martin, P. J., Hacker, B. M., . . . Wolf, F. M. (2014). Expanding assessments of translational research programs: Supplementing metrics with value judgments. Evaluation & the Health Professions, 37(1), 83-97.
Udovic, D., Morris, D., Dickman, A., Postlethwait, J., & Wetherwax, P. (2002). Workshop biology: Demonstrating the effectiveness of active learning in an introductory biology course. BioScience, 52(3), 272-281.
Viswanathan, M., Ammerman, A., Eng, E., Gartlehner, G., Lohr, K. N., Griffith, D., . . . Whitener, L. (2004). Community-based participatory research: Assessing the evidence: Summary (Evidence Report/Technology Assessment No. 99). Rockville, MD: Agency for Healthcare Research and Quality.
Westfall, J. M., Mold, J., & Fagnan, L. (2007). Practice-based research: ‘Blue Highways’ on the NIH roadmap. Journal of the American Medical Association, 297(4), 403-406.
Wood, W. B. (2009). Innovations in teaching undergraduate biology and why we need them. Annual Review of Cell and Developmental Biology, 25, 93-112.
Woolf, S. H. (2008). The meaning of translational research and why it matters. Journal of the American Medical Association, 299(2), 211-213.
Received 30 August 2016 | Accepted 10 September 2016 | Published 7 November 2016
Copyright © 2016 Journal of Research Practice and the authors